Treatment of Gangrene Wounds with Hydrocolloid Dressing Methods for Diabetes Mellitus Type 2 in Educational Hospital North Sumatera University
https://doi.org/10.33860/jik.v19i1.3846
Keywords:
Gangrene wound care, modern hydrocolloid dressing, Diabetes MellitusAbstract
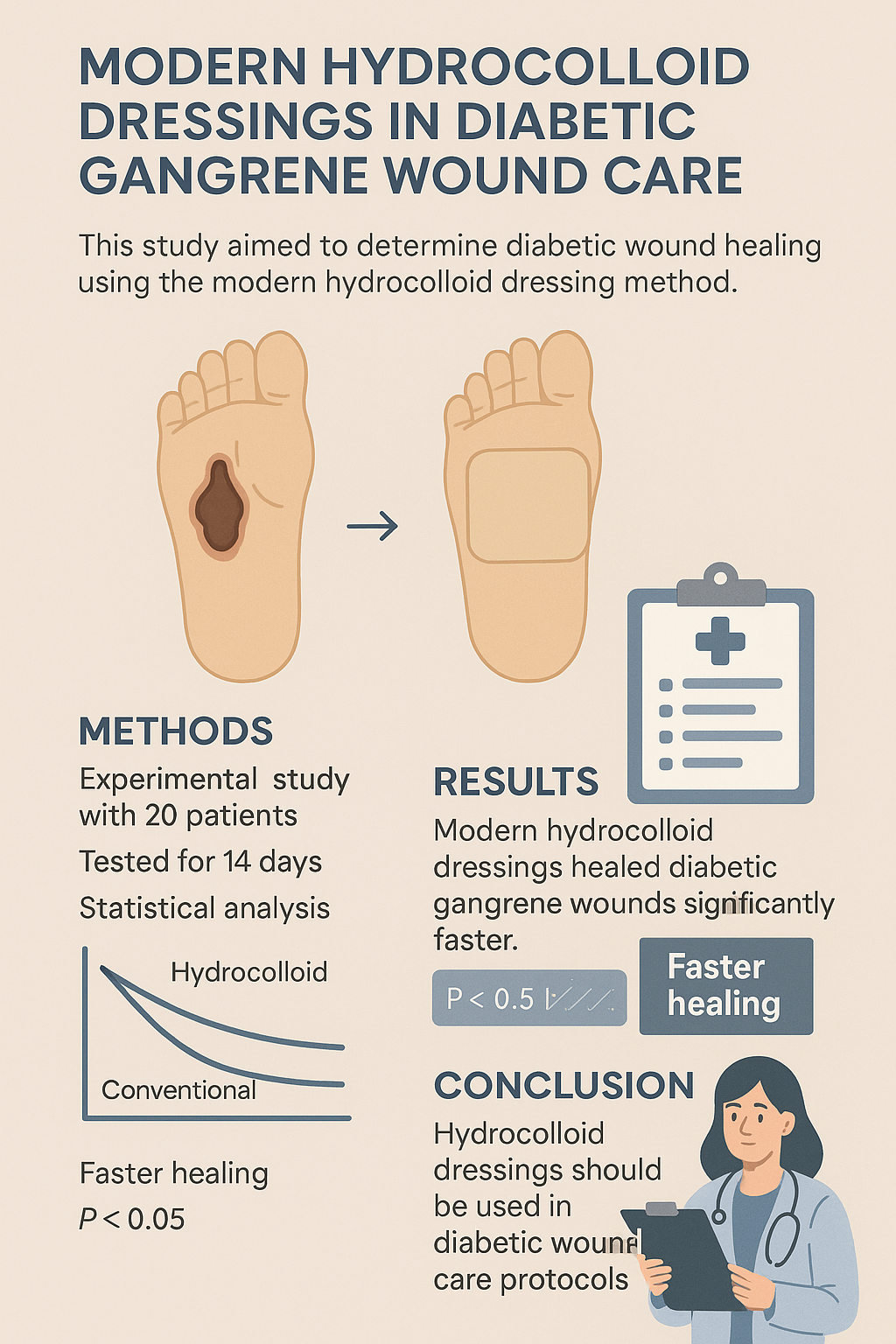
Wound care in a moist environment is superior to a dry environment. Appropriate wound care methods can help accelerate the healing of gangrenous wounds. This study aimed to determine diabetic wound healing using the modern hydrocolloid dressing method. This experimental research design utilized pre-test and post-test techniques to assess the difference in the effect of gangrene wound care with modern hydrocolloid dressings on gangrene wound healing in diabetic patients. The study was conducted at USU Teaching Hospital Medan for 14 days, involving 20 respondents with Type II DM patients experiencing gangrene wounds, obtained through non-probability sampling. Data analysis was performed using the independent t-test. The results showed a significant difference in gangrene wound care with the modern hydrocolloid dressing method (p < 0.05). The modern hydrocolloid dressing method led to faster healing of gangrene wounds. Conclusion: respondents who used the modern hydrocolloid dressing method experienced better wound status development and faster healing. It is expected that hospitals will plan and establish SOPs for wound care in DM patients with gangrene using modern hydrocolloid dressings and reduce the use of conventional methods. These implications highlight the importance of implementing modern methods in wound care protocols for patients with diabetes mellitus with gangrene, mainly to prevent amputation and improve patients' quality of life. Recommendations include the implementation of modern wound care SOPs, training for health workers, patient and family education, further research, and the procurement of modern dressings.
References
1. Perkeni. Pedoman Pengelolaan Dan Pencegahan Diabetes Melitus Tipe 2 Dewasa Di Indonesia. Soebagijo SA, editor. Jakarta: PB PERKENI; 2021. 5 p.
2. WHO. World Health Statistic. New York; 2019.
3. Rosyid. Etiology, pathophysiology, diagnosis and management of diabetics’ foot ulcer. Int J Res Med Sci. 2017;5(10).
4. Nuutila, Erikson. Moist Wound Healing with Commonly Available Dressings. Advances in Wound Care. Adv Wound Care (New Rochelle). 2021;10(12).
5. Barbu A, Neamtu B, Zăhan M, Iancu GM, Bacila C, Mireșan V. Current trends in advanced alginate-based wound dressings for chronic wounds. J Pers Med. 2021;11(9).
6. Weledji EP, Fokam P. Treatment of the diabetic foot-to amputate or not? BioMed Cent [Internet]. 2014 [cited 2024 Aug 7]; Available from: http://www.biomedcentral.com/1471-2482/14/83
7. Tan ST, Winarto N, Dosan R, Aisyah PB. The Benefits Of Occlusive Dressings In Wound Healing. Open Dermatol J. 2019 Jun 19;13(1):27–33.
8. Baranoski S, Ayello EA. Wound Care Essentials: Practice Principles. 5th ed. Philadelphia: Lippincott Williams & Wilkins (LWW); 2020.
9. Walker, Gillespie, Thalib, Higgins, Whitty. Foam dressings for treating pressure ulcers. Cochrane Database of Systematic Reviews. Cochrane Database Syst Rev. 2017;10(1).
10. Dhivya, Padma, Shantini. Wound dressings - A review. Biomed. 2018;5(4).
11. Hastuti. Faktor-Faktor Risiko Ulkus Diabetika pada Penderita Diabetes mellitus, (Studi Kasus di RSUD. Dr. Moewardi Surakarta). Sebelas Maret; 2019.
12. ADA. American Diabetes Association. Standards of Medical Care in Diabetes-2017. J Clin Appl Res Educ. 2017;40(1):S1-135.
13. Kamalarathnam, Varadarajan. Diabetic peripheral neuropathy in diabetic patients attending an urban health and training centre. J Fam Med Prim Care. 2022;11(12).
14. Teodorescu, Vavra, Kibbe. Peripheral arterial disease in women. J Vasc Surg. 2018;57(4).
15. Jiang, Chen, Li. Effectiveness of picture description education on compliance behaviors of diabetics in western Sichuan district. Int J Nurs Sci. 2018;3(3).
16. Adiewere, Gillis, Jiwani I, Meal, Shaw, Adams. A systematic review and meta-analysis of patient education in preventing and reducing the incidence or recurrence of adult diabetes foot ulcers (DFU). Heliyon. 2018;4(5).
17. Roy, Zayas, Singh SK, Delgado K, Wood SJ, Mohamed MF, et al. Overriding impaired FPR chemotaxis signaling in diabetic neutrophil stimulates infection control in murine diabetic wound. ELife. Elife. 2022;11(3).
18. Barbu, Neamtu, Zahan, Iancu, Bacila, Miresan. Current trends in advanced alginate-based wound dressings for chronic wounds. J Pers Med. 2021;11(9).
19. Alrub AA, Hyassat D, Khader YS, Bani-Mustafa R, Younes N, Ajlouni K. Factors Associated with Health-Related Quality of Life amongJordanian Patients with Diabetic Foot Ulcer. J Diabetes Res. 2019;
20. Yedjou CG, Grigsby J, Mbemi A, Nelson D, Mildort B, Latinwo L, et al. The Management of Diabetes Mellitus Using Medicinal Plants and Vitamins. Int J Mol Sci. 2023;24(10).
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with Poltekita : Jurnal Ilmu Kesehatan agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-ShareAlike 2.0 Generic License.
Poltekita : Jurnal Ilmu Kesehatan is licensed under a Creative Commons Attribution-Share Alike 4.0 International License
You are free to:
- Share, copy and redistribute the material in any medium or format
- Adapt, remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.






