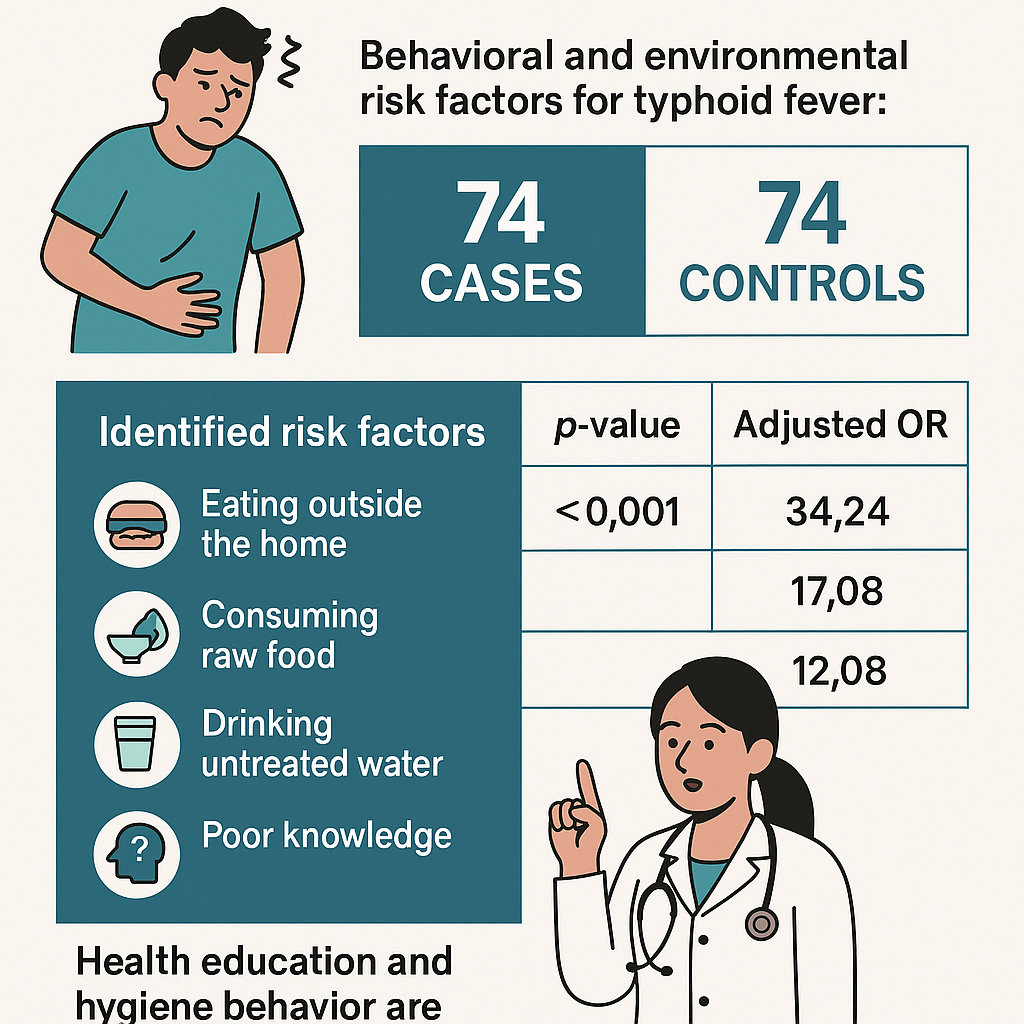
Behavioral and Environmental Risk Factors of Typhoid Fever: A Case-Control Study in Balongpanggang, Gresik Regency
https://doi.org/10.33860/jik.v19i1.4171
Keywords:
Typhoid fever;, behavioral risk factors, public health, hygiene practices, food and water safety, case control studyAbstract
Typhoid fever remains a significant public health burden in developing countries, including Indonesia, where poor hygiene and sanitation contribute to its endemicity. This study aimed to identify behavioral risk factors associated with typhoid fever in the working area of UPT Puskesmas Balongpanggang, Gresik Regency. A quantitative, analytic case control study was conducted involving 74 respondents, equally divided between the case group (patients diagnosed with typhoid fever) and the control group (individuals without the disease). Purposive sampling was applied to select participants, and data collection was carried out through structured interviews using a validated questionnaire. Statistical analysis was performed using chi square tests to evaluate associations between specific behaviors and disease occurrence. The study identified six significant behavioral risk factors: eating outside the home (OR = 5.022; 95% CI: 1.465–17.217), consuming raw food (OR = 15.231; 95% CI: 1.850–125.420), drinking untreated water (OR = 10.828; 95% CI: 3.182–36.848), poor knowledge about typhoid (OR = 90.417; 95% CI: 16.991–481.135), family history of typhoid (OR = 4.758; 95% CI: 1.720–13.164), and not washing hands after defecation (OR = 36.458; 95% CI: 7.491–177.444). These results emphasize the role of individual hygiene practices and household behaviors in typhoid transmission. In conclusion, this study provides strong evidence for prioritizing behavior focused public health interventions and educational programs as key strategies for typhoid fever prevention in endemic communities.
References
1. Giri S, Mohan VR, Srinivasan M, Kumar N, Kumar V, Dhanapal P, et al. Case-Control Study of Household and Environmental Transmission of Typhoid Fever in India. The Journal of Infectious Diseases. 2021;224(Supplement_5):S584–92. Available from: https://pubmed.ncbi.nlm.nih.gov/35238355/
2. Taha AM, Abouelmagd K, Mahmoud AM, Elkasaby MH, Nguyen D, Ahmed R, et al. Safety and Immunogenicity of Vi-Diphtheria Toxoid Typhoid Conjugate Vaccine Among Children Below 2 years: A Systematic Review and Meta-Analysis. Frontiers in Microbiology. 2024;15. Available from: https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1385834/full
3. Brockett S, Wolfe MK, Hamot A, Appiah GD, Mintz ED, Lantagne D. Associations Among Water, Sanitation, and Hygiene, and Food Exposures and Typhoid Fever in Case–Control Studies: A Systematic Review and Meta-Analysis. American Journal of Tropical Medicine and Hygiene. 2020;103(3):1020–31. Available from: https://pubmed.ncbi.nlm.nih.gov/32700668/
4. Gauld J, Olgemoeller F, Nkhata R, Li C, Chirambo AC, Morse T, et al. Domestic River Water Use and Risk of Typhoid Fever: Results From a Case-Control Study in Blantyre, Malawi. Clinical Infectious Diseases. 2019;70(7):1278–84. Available from: https://doi.org/10.1093/cid/ciz405
5. Jenkins A, Jupiter SD, Jenney A, Rosa V, Naucukidi A, Prasad N, et al. Environmental Foundations of Typhoid Fever in the Fijian Residential Setting. International Journal of Environmental Research and Public Health. 2019;16(13):2407. Available from: https://doi.org/10.3390/ijerph16132407
6. Paputungan W. Hubungan antara perilaku hidup bersih dan sehat dengan kejadian demam tifoid di wilayah kerja puskesmas upai kota kotamobagu tahun 2015. Pharmacon. 2016;5(2). Available from: https://ejournal.unsrat.ac.id/v3/index.php/pharmacon/article/view/12215
7. Mulu W, Genet C, Ababu K, Getachew S, Tesfaye F, Wube A, et al. Seroconfirmed Typhoid Fever and Knowledge, Attitude, and Practices Among Febrile Patients Attending at Injibara General Hospital, Northwest Ethiopia. Biomed Research International. 2021;2021(1). Available from: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1357131/full
8. Phillips MT, Antillón M, Bilcke J, Bar‐Zeev N, Limani F, Debellut F, et al. Cost-Effectiveness Analysis of Typhoid Conjugate Vaccines in an Outbreak Setting: A Modeling Study. BMC Infectious Diseases. 2023;23(1). Available from: https://doi.org/10.1186/s12879-023-08105-2
9. Yousafzai MT, Qamar FN, Shakoor S, Saleem K, Lohana H, Karim SMM, et al. Ceftriaxone-ResistantSalmonellaTyphi Outbreak in Hyderabad City of Sindh, Pakistan: High Time for the Introduction of Typhoid Conjugate Vaccine. Clinical Infectious Diseases. 2019;68(Supplement_1):S16–21. Available from: https://pubmed.ncbi.nlm.nih.gov/30767003/
10. Abayneh M, Aberad M, Habtemariam Y, Alemu Y. Health Facility-Based Prevalence of Typhoid Fever, Typhus and Malaria Among Individuals Suspected of Acute Febrile Illnesses in Southwest Region, Ethiopia. Frontiers in Epidemiology. 2024;4. Available from: https://www.frontiersin.org/journals/epidemiology/articles/10.3389/fepid.2024.1391890/full?utm_source
11. Walker JW, Chaguza C, Grubaugh ND, Carey ME, Baker S, Khan K, et al. Assessing the Global Risk of Typhoid Outbreaks Caused by Extensively Drug Resistant Salmonella Typhi. Nature Communications. 2023;14(1). Available from: https://www.researchgate.net/publication/374761937_Assessing_the_global_risk_of_typhoid_outbreaks_caused_by_extensively_drug_resistant_Salmonella_Typhi
12. Stanaway JD, Reiner RC, Blacker BF, Goldberg EM, Rahim F, Troeger C, et al. The Global Burden of Typhoid and Paratyphoid Fevers: A Systematic Analysis for the Global Burden of Disease Study 2017. The Lancet Infectious Diseases. 2019;19(4):369–81. Available from: https://pubmed.ncbi.nlm.nih.gov/30792131/
13. Gauld J, Olgemoeller F, Heinz E, Nkhata R, Bilima S, Wailan AM, et al. Spatial and Genomic Data to Characterize Endemic Typhoid Transmission. Clinical Infectious Diseases. 2021;74(11):1993–2000. Available from: https://pubmed.ncbi.nlm.nih.gov/34463736/
14. Kim S, Lee KS, Pak GD, Excler J, Sahastrabuddhe S, Marks F, et al. Spatial and Temporal Patterns of Typhoid and Paratyphoid Fever Outbreaks: A Worldwide Review, 1990–2018. Clinical Infectious Diseases. 2019;69(Supplement_6):S499–509. Available from: https://www.researchgate.net/publication/336924091_Spatial_and_Temporal_Patterns_of_Typhoid_and_Paratyphoid_Fever_Outbreaks_A_Worldwide_Review_1990-2018
15. Laidlow TA, Stafford R, Jennison AV, Bell RH, Graham R, Graham T, et al. A Multi‐jurisdictional Outbreak of Salmonella Typhimurium Infections Linked to Backyard Poultry—Australia, 2020. Zoonoses and Public Health. 2022;69(7):835–42. Available from: https://www.researchgate.net/publication/361738734_A_multi-jurisdictional_outbreak_of_Salmonella_Typhimurium_infections_linked_to_backyard_poultry-Australia_2020
16. Slamet JS. Kesehatan Lingkungan.Revisi. Gadjah Mada University Press. 2018; Available from: https://www.scribd.com/document/444072483/Jurnal-Kesehatan-Lingkungan?utm_source
17. Seran ER, Palandeng H, Kallo V. Hubungan Personal Hygiene dengan Kejadian Demam Tifoid di Wilayah Kerja Puskesmas Tumaratas. Ejournal Keperawatan (e-Kp). 2015;3(2):1–8. Available from: https://ejournal.unsrat.ac.id/v3/index.php/jkp/article/view/7449?utm_source
18. Furqan M. Nomor 1. Maret 2023 Jurnal Sains Terapan Pariwisata Halaman. 8:30–41. Available from: https://www.researchgate.net/publication/369524284_Persepsi_Pengunjung_tentang_Hygiene_Makanan_Sala_di_Ulakan_Padang_Pariaman
19. Gunawan A, Rahman IA, Nurapandi A, Maulana NC. Hubungan Personal Hygiene dengan Kejadian Demam Typhoid pada Remaja di Wilayah Kerja Puskesmas Imbanagara Kabupaten Ciamis. Healthcare Nursing Journal [Internet]. 2022;4(2):404–12. Available from: https://jurnal.unigal.ac.id/index.php/hnj/article/view/7079
20. Notoatmodjo S. Metodologi Kesehatan Kesehatan. Rineka Cipta: Jakarta. 2017; Available from: https://www.belbuk.com/metodologi-penelitian-kesehatan/produk/1831?utm_source
21. Nuruzzaman H, Syahrul F. Analisis risiko kejadian demam tifoid berdasarkan kebersihan diri dan kebiasaan jajan di rumah. Jurnal Berkala Epidemiologi. 2016;4(1):74–86. Available from: https://www.researchgate.net/publication/324449671_Risk_Analysis_of_Typhoid_Fever_Based_on_Personal_Hygiene_and_Street_Food_Consumption_Habit_at_Home
Downloads
Published
How to Cite
Issue
Section
License
Authors who publish with Poltekita : Jurnal Ilmu Kesehatan agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-ShareAlike 2.0 Generic License.
Poltekita : Jurnal Ilmu Kesehatan is licensed under a Creative Commons Attribution-Share Alike 4.0 International License
You are free to:
- Share, copy and redistribute the material in any medium or format
- Adapt, remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.