Involvement of Community Organisations in Providing Information, Motivation to TB Patients to Adhere to Regular Treatment
https://doi.org/10.33860/bpk.v53i2.4056
Keywords:
Involvement, Community Organizations, IMB, Adherence, TuberculosisAbstract
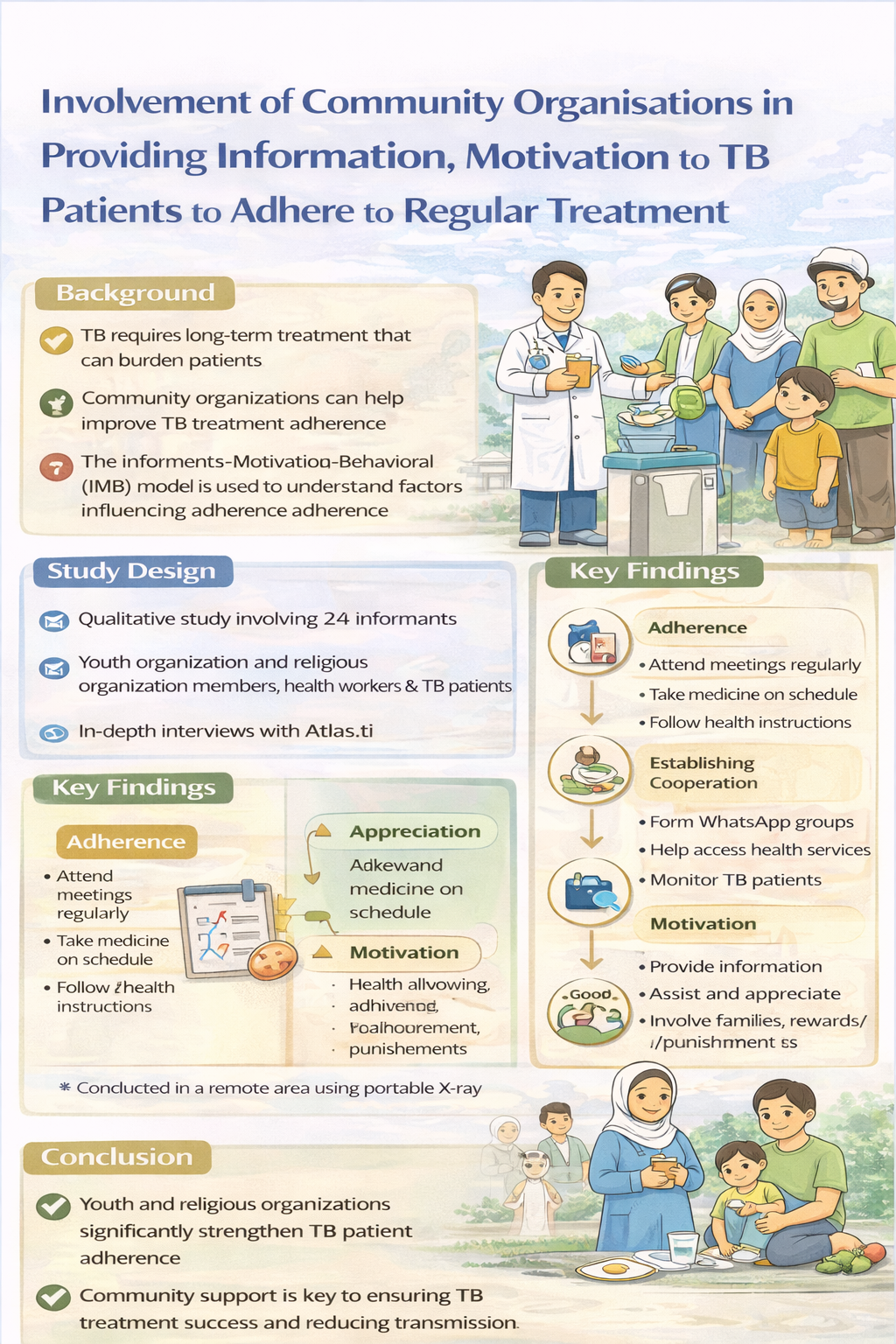
Background: Tuberculosis (TB) requires long-term treatment, and non-adherence remains a major challenge that increases the risk of treatment failure and disease transmission. The Information–Motivation–Behavioral (IMB) model highlights the importance of social support in improving adherence. Community-based organizations, particularly youth and religious organizations, are deeply embedded in society and have the potential to support TB patients through information dissemination and motivational assistance. This study aimed to explore the role of community organizations in providing information and motivation to enhance treatment adherence among TB patients.
Methods: A qualitative study with a phenomenological approach was conducted in the Serdang Bedagai health service area, North Sumatra, Indonesia. A total of 24 informants, including health workers, members of youth and religious organizations, and TB patients, were recruited using purposive sampling. Data were collected through in-depth interviews and analyzed using qualitative content analysis supported by Atlas.ti software.
Results: Three main themes emerged: adherence to treatment, establishment of cooperation, and motivation. Community organizations supported adherence by facilitating regular meetings, assisting medication intake, establishing communication groups, and providing emotional, informational, and family support.
Conclusion: The involvement of youth and religious organizations plays a critical role in strengthening TB treatment adherence. Integrating community-based support with health services may enhance motivation, supervision, and long-term treatment compliance among TB patients.
Downloads
References
Balay, G., Abdella, K., Kebede, W., Tadesse, M., Bonsa, Z., Mekonnen, M., Amare, M., & Abebe, G. (2024). Resistance to pyrazinamide in Mycobacterium tuberculosis complex isolates from previously treated tuberculosis cases in Southwestern Oromia, Ethiopia. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 34. https://doi.org/10.1016/j.jctube.2023.100411
Bonsa, Z., Tadesse, M., Balay, G., Kebede, W., & Abebe, G. (2024). Discordance between genotypic and phenotypic methods for the detection of rifampicin and isoniazid resistant Mycobacterium tuberculosis and the correlation with patient treatment outcomes. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 34. https://doi.org/10.1016/j.jctube.2023.100410
Bruzadelli Paulino da Costa, F., Zamboni Berra, T., Garcia de Almeida Ballestero, J., Bartholomay Oliveira, P., Maria Pelissari, D., Mathias Alves, Y., Carlos Vieira Ramos, A., Queiroz Rocha de Paiva, J., Kehinde Ayandeyi Teibo, T., & Alexandre Arcêncio, R. (2023). Treatment of drug-resistant tuberculosis in children and young adolescents in Brazil. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 33. https://doi.org/10.1016/j.jctube.2023.100388
Feng, P. J. I., Horne, D. J., Wortham, J. M., & Katz, D. J. (2023). Trends in tuberculosis clinicians’ adoption of short-course regimens for latent tuberculosis infection. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 33. https://doi.org/10.1016/j.jctube.2023.100382
Friedena, T. R., & Sbarbarob, J. A. (2007). Promoting adherence to treatment for tuberculosis: The importance of direct observation. In Bulletin of the World Health Organization (Vol. 85, Issue 5, pp. 407–409). https://doi.org/10.2471/BLT.06.038927
Fu, L., Zhang, X., Xiong, J., Sun, F., Weng, T., Li, Y., Zhang, P., Li, H., Yang, Q., Cai, Y., Liang, H., Chen, Q., Wang, Z., Liu, L., Chen, X., Zhang, W., & Deng, G. (2023). Selecting an appropriate all-oral short-course regimen for patients with multidrug-resistant or pre-extensive drug-resistant tuberculosis in China: A multicenter prospective cohort study. International Journal of Infectious Diseases, 135, 101–108. https://doi.org/10.1016/j.ijid.2023.08.001
Getahun, G. K., Gezahegn, E., Endazenawe, G., Shitemaw, T., Negash, Z., & Dessu, S. (2023). Survival status and risk factors for mortality among multidrug-resistant tuberculosis patients in Addis Ababa, Ethiopia: A retrospective follow-up study. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 33. https://doi.org/10.1016/j.jctube.2023.100398
Igwaran, A., & Edoamodu, C. E. (2021). Bibliometric analysis on tuberculosis and tuberculosis-related research trends in Africa: A decade-long study. Antibiotics, 10(4). https://doi.org/10.3390/antibiotics10040423
Izudi, J., Okello, G., & Bajunirwe, F. (2023). Low treatment success rate among previously treated persons with drug-susceptible pulmonary tuberculosis in Kampala, Uganda. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 32. https://doi.org/10.1016/j.jctube.2023.100375
Kavanagh, M. M., Gostin, L. O., & Stephens, J. (2020). Tuberculosis, human rights, and law reform: Addressing the lack of progress in the global tuberculosis response. PLoS Medicine, 17(10). https://doi.org/10.1371/journal.pmed.1003324
Kilale, A. M., Pantoja, A., Jani, B., Range, N., Ngowi, B. J., Makasi, C., Majaha, M., Manga, C. D., Haule, S., Wilfred, A., Hilary, P., Mahamba, V., Nkiligi, E., Muhandiki, W., Matechi, E., Mutayoba, B., Nishkiori, N., & Ershova, J. (2022). Economic burden of tuberculosis in Tanzania: a national survey of costs faced by tuberculosis-affected households. BMC Public Health, 22(1). https://doi.org/10.1186/s12889-022-12987-3
Lee, J., Kim, D., Hwang, J., & Kwon, J.-W. (2024). Incidence of tuberculosis (TB) disease in individuals diagnosed with TB infection following screening: a population-based cohort study in South Korea. International Journal of Infectious Diseases. https://doi.org/10.1016/j.ijid.2024.02.004
Mccormick, C. L. (2017). Gaps Of Tuberculosis: A Review Of The Literature Surrounding The Diagnosis, Prognosis, Treatment, And Prevention Of Tuberculosis.
Nabisere-Arinaitwe, R., Namatende-Sakwa, L., Bayiga, J., Nampala, J., Alinaitwe, L., Aber, F., Otaalo, B., Musaazi, J., King, R., Kesby, M., Sloan, D. J., & Sekaggya-Wiltshire, C. (2023). “It is not easy”: Experiences of people living with HIV and tuberculosis on Tuberculosis treatment in Uganda. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 33. https://doi.org/10.1016/j.jctube.2023.100385
Nguyen, T. M. P., Le, T. H. M., Merle, C. S. C., Pedrazzoli, D., Nguyen, N. L., Decroo, T., Nguyen, B. H., Hoang, T. T. T., & Nguyen, V. N. (2023). Effectiveness and safety of bedaquiline-based, modified all-oral 9–11-month treatment regimen for rifampicin-resistant tuberculosis in Vietnam. International Journal of Infectious Diseases, 126, 148–154. https://doi.org/10.1016/j.ijid.2022.11.007
Putra, K. W. R., & Toonsiri, C. (2019). FACTORS RELATED TO THE SUCCESSFUL TREATMENT OF TUBERCULOSIS: A LITERATURE REVIEW. Belitung Nursing Journal, 5(4), 136–146. https://doi.org/10.33546/bnj.749
Rahmati, S., Nasehi, M., Bahrampour, A., Mirzazadeh, A., & Shahesmaeili, A. (2023). Barriers and gaps in tuberculosis care and treatment in Iran: A multi-center qualitative study. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 31. https://doi.org/10.1016/j.jctube.2023.100353
Rudgard, W. E., Evans, C. A., Sweeney, S., Wingfield, T., Lönnroth, K., Barreira, D., & Boccia, D. (2017). Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study. PLoS Medicine, 14(11). https://doi.org/10.1371/journal.pmed.1002418
Wagnew, F., Alene, K. A., Kelly, M., & Gray, D. (2023). The effect of undernutrition on sputum culture conversion and treatment outcomes among people with multidrug-resistant tuberculosis: a systematic review and meta-analysis. International Journal of Infectious Diseases, 127, 93–105. https://doi.org/10.1016/j.ijid.2022.11.043
Yang, J. J., Goff, A., Wild, D. J., Ding, Y., Annis, A., Kerber, R., Foote, B., Passi, A., Duerksen, J. L., London, S., Puhl, A. C., Lane, T. R., Braunstein, M., Waddell, S. J., & Ekins, S. (2024). Computational drug repositioning identifies niclosamide and tribromsalan as inhibitors of Mycobacterium tuberculosis and Mycobacterium abscessus. Tuberculosis, 146, 102500. https://doi.org/10.1016/j.tube.2024.102500
Yulianti Sutrisno, R., Rossytalia Widiyastuti, D., Wahyu Setyo Budi, A., Tesma Wulandari, B., Irawati, K., Suanrueang, P., & Author, C. (2022). Patient Experience in The Healing Process of Tuberculosis: A Phenomenology Study. IJNP (Indonesian Journal of Nursing Practices, 6(1), 57–64. https://doi.org/10.18196/ijnp.v6i1.15662
Zeding, Z., Liu, L., Wang, C., Tian, Q., Zhang, J. Q., Zen, Y., Zhang, N., Shen, J., Na A, M., BaSang, P. C., Lv, X. M., Yang, S. L., Meng, S. Y., & Yang, L. H. (2023). A retrospective analysis of 25 cases of Addison’s disease caused by adrenal tuberculosis in Tibet and review of related literature. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 31. https://doi.org/10.1016/j.jctube.2023.100358
Zenatti, G., Raviglione, M., Tesfaye, F., Bobosha, K., Björkman, P., & Walles, J. (2023). High variability in tuberculosis treatment outcomes across 15 health facilities in a semi-urban area in central Ethiopia. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases, 30. https://doi.org/10.1016/j.jctube.2022.100344