The Effectiveness of Sound Stimulators as a Means of Monitoring Fetal Well-Being at the Gatot Soebroto Army Central Hospital
https://doi.org/10.33860/jbc.v7i1.3861
Keywords:
fetal sleep, fetal well-being monitoring, InnovationAbstract
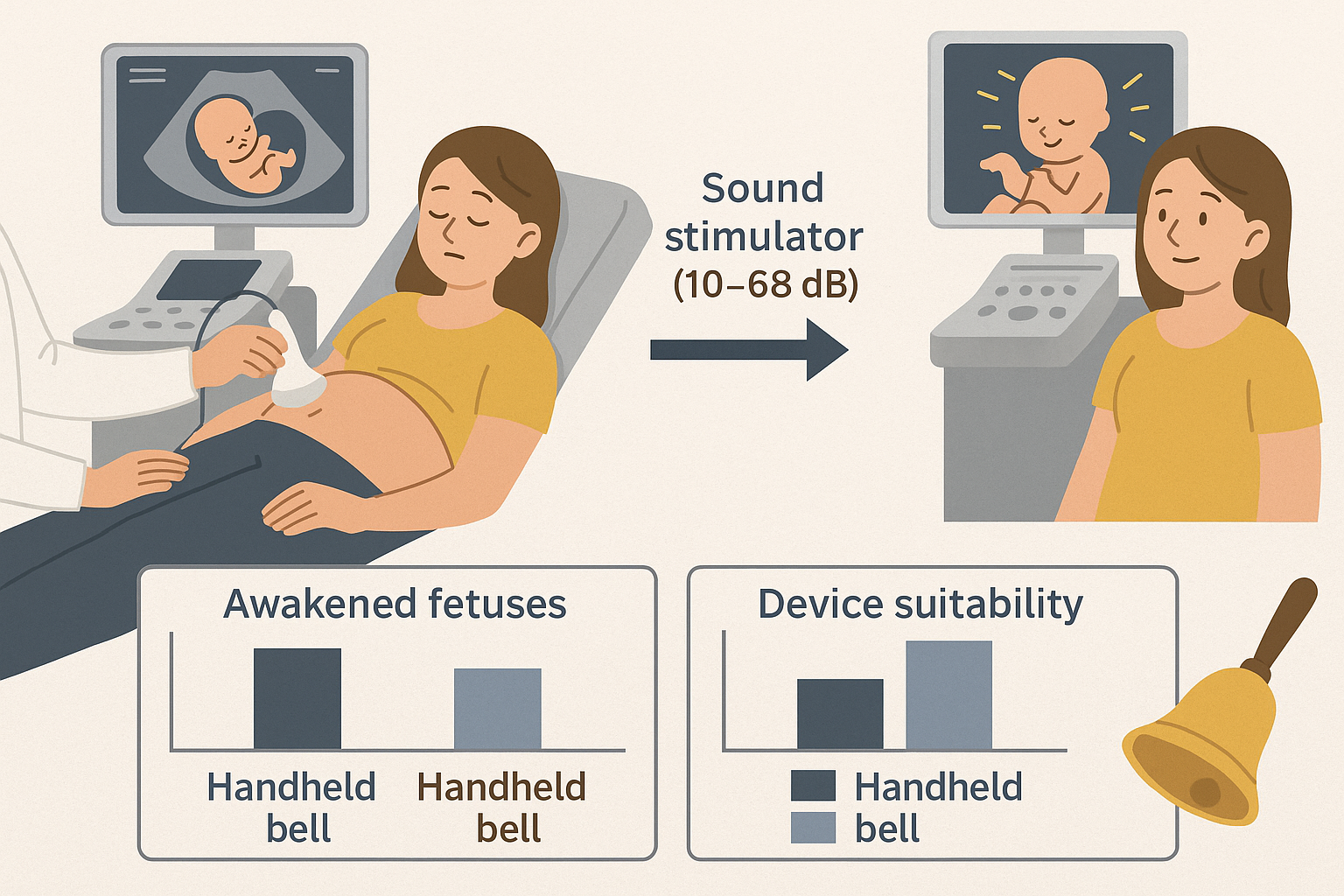
Introduction: Fetal inactivity during well-being monitoring can stem from sleep rather than distress. This study assessed a sound stimulator, a vibroacoustic device using digital speaker-emitted sound waves, against the traditional klenengan bell for awakening sleeping fetuses. Objective: The aim was to assess the stimulator's effectiveness in awakening sleeping fetuses and to verify its proper usage by operators. Methods: The intervention group received the sound stimulator, emitting a consistent decibel level (10-68 dB) via a speaker placed near the fetal head for approximately one minute. A quantitative, posttest-only study design was employed at Gatot Soebroto Army Central Hospital, involving 60 participants. Ethical approval was granted by the Institute of Health Research Ethics Committee of Dharma Husada College of Health Sciences (No. 13/KEPK/SDHB/B/V/2023). Results: The sound stimulator successfully awakened 27 of 30 sleeping fetuses within 30 seconds. Device suitability was high, with 29 of 30 deemed appropriate and 27 achieving noise levels below 68 dB, prioritizing safety and comfort. Conclusion: Wilcoxon Signed Rank test results (Asymp.sig = 0.035) confirmed the stimulator's effectiveness. The innovative sound stimulator was superior to the klenengan bell. It provides a practical, efficient, and safe tool (noise levels <68 dB) for fetal welfare monitoring
Downloads
References
Curran, M. A. (2019). Fetal development. Retrieved June 24, 2024, from perinatology.com website: https://perinatology.com/Reference/Fetal%20development.htm
Endjun, J. J. (2018). Basic obstetric and gynecologic ultrasound for physicians. Bandung: Adia. http://repository.stikesrspadgs.ac.id/556/1/PPK%20USG%20OBGIN%20DASAR%20%28e-book%202020%29.pdf
Vitale, F. M., Chirico, G., & Lentini, C. (2021). Sensory stimulation in the NICU environment: Devices, systems, and procedures to protect and stimulate premature babies. Children, 8(5), 334. https://pubmed.ncbi.nlm.nih.gov/33923031/
Hussain, N. M., O’Halloran, M., McDermott, B., & Elahi, M. A. (2024). Fetal monitoring technologies for the detection of intrapartum hypoxia-challenges and opportunities. Biomedical Physics & Engineering Express, 10(2), 022002. https://pubmed.ncbi.nlm.nih.gov/38118183/
Hutton, E.K. & Murray-Davis, B. (2024). Comprehensive Midwifery: The Role of the Midwife in Health Care Practice, Education, and Research. https://nmoer.pressbooks.pub/cmroleofmidwifery2/
Indonesian Ministry of Health. (2021). Indonesia Health Profile 2020. https://kemkes.go.id/id/profil-kesehatan-indonesia-2021
Ibrahim, H. A., Elgzar, W. T., & Saied, E. A. (2021). The effect of different positions during non-stress test on maternal hemodynamic parameters, satisfaction, and fetal cardiotocographic patterns. African journal of reproductive health, 25(1), 81-89. https://www.bioline.org.br/pdf?rh21010
Jia, Y. J., Ghi, T., Pereira, S., Perez-Bonfils, A. G., & Chandraharan, E. (2023). Pathophysiological interpretation of fetal heart rate tracings in clinical practice. American Journal Of Obstetrics And Gynecology, 228(6), 622-644. https://pubmed.ncbi.nlm.nih.gov/37270259/.
Kemenkes RI. (2018). Healthy portrait of Indonesia in 2018. Jakarta. https://sehatnegeriku.kemkes.go.id/baca/umum/20181102/0328464/potret-sehat-indonesia-riskesdas-2018/
Lee, L., Chang, Y. H., Liang, W. J., & Huang, Y. C. (2022). The effect of music intervention on fetal education via doppler fetal monitor. Children, 9(6), 918. https://pubmed.ncbi.nlm.nih.gov/35740853/
Lemma, K., Misker, D., Kassa, M., Abdulkadir, H., & Otayto, K. (2022). Determinants of birth asphyxia among newborn live births in public hospitals of Gamo and Gofa zones, Southern Ethiopia. BMC pediatrics, 22(1), 280. https://pubmed.ncbi.nlm.nih.gov/35562670/
Maeda, K., and M, T. (2017). Fetal Response to Sound and Light: Possible Fetal Education? Journal of Neonatal Biology, 06(01), 1-2. https://doi.org/10.4172/2167-0897.1000247. https://www.walshmedicalmedia.com/open-access/fetal-response-to-sound-and-light-possible-fetal-education-2167-0897-1000247.pdf
Mangesi, L., Hofmeyr, G. J., Smith, V., and Smyth, R. M. D. (2015). Fetal movement counting for assessment of fetal wellbeing. Cochrane Database of Systematic Reviews, 2015(10). https://pubmed.ncbi.nlm.nih.gov/26467769/
Marx, V., and Nagy, E. (2015). Fetal behavioral responses to maternal voice and touch. PLoS ONE, 10(6), 1-15. https://doi.org/10.1371/journal.pone.0129118.
Movalled, K., Sani, A., Nikniaz, L., & Ghojazadeh, M. (2023). The impact of sound stimulations during pregnancy on fetal learning: a systematic review. BMC pediatrics, 23(1), 183. https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-023-03990-7
More, A., Thorat, M. S., Desai, S., Mahadik, R. V., Kharge, G. V., & Deshmukh, M. D. (2024) Measuring Efficiency and Effectiveness in Public Health Management: Methodologies and Applications, 23(1), 63-75. https://www.seejph.com/index.php/seejph/article/view/488
Newton, E. R., and May, L. (2017). Adaptation of Maternal-Fetal Physiology to Exercise in Pregnancy: The Basis of Guidelines for Physical Activity in Pregnancy. Clinical Medicine Insights: Women's Health, 10, 1179562X1769322. https://doi.org/10.1177/1179562x17693224.
NHS. (2023) The Pregnancy Book: Your complete guide to a healthy pregnancy, labour and childbirth. https://www.publichealth.hscni.net/sites/default/files/2023-06/Preg%20book%202023%20complete.pdf
Pirhadi, M. (2015). The effect of vibroacoustic stimulation and music on fetal movement. International Journal of Pediatrics, 3(5), 903-908. https://doi.org/10.22038/ijp.2015.4857. https://jpp.mums.ac.ir/article_4857_3bb504505df0a57199995bf0360ede05.pdf
Singh, K., and Das, C. (2015). Role of vibroacoustic stimulation test in prediction of fetal outcome in terms of Apgar score. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 4(5), 1427-1430. https://www.ijrcog.org/index.php/ijrcog/article/view/2147
Toker, E., & Gökduman Keleş, M. (2024). The effect of virtual reality on fetal movement, fetal heart rate, maternal satisfaction, fatigue, and anxiety levels and vital signs of pregnant women during non-stress test: A randomized controlled trial. Health Care for Women International, 45(7), 765-781. https://pubmed.ncbi.nlm.nih.gov/37347556/.
UNICEF Indonesia. (2020). The situation of children in Indonesia. UNICEF Indonesia, 1-66. Retrieved from https://www.unicef.org/indonesia/media/5291/file/Situasi Children in Indonesia.pdf.
Vitale, F. M., Chirico, G., & Lentini, C. (2021). Sensory stimulation in the NICU environment: Devices, systems, and procedures to protect and stimulate premature babies. Children, 8(5), 334. https://pubmed.ncbi.nlm.nih.gov/33923031/
Yetkin, A. K., Güneş, B., & Erbaş, O. (2023). Prenatal Auditory Stimulation and Its Significance for Newborns. Journal of Experimental and Basic Medical Sciences, 4(2), 096-103. https://jebms.org/full-text/138
Zbelo, M. G. (2024). Fetal Heart Rate Self-Monitoring by Mothers in Labor (Doctoral dissertation, Walden University). https://scholarworks.waldenu.edu/dissertations/16139/
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Teni Nurlatifah H.R., May Rhismayati, Hidayat Wijayanegara (Author)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors who publish with Jurnal Bidan Cerdas agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-Share Alike 4.0 International License
You are free to:
- Share, copy and redistribute the material in any medium or format
- Adapt, remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.




